Wastewater surveillance for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has gained global visibility as a powerful public health tool for disease prevention and management.
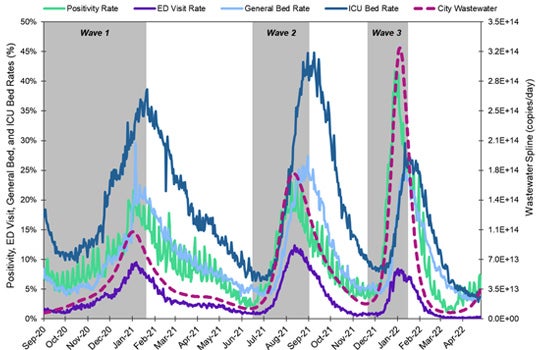
Multi-institutional efforts to integrate and evaluate a citywide surveillance system in Houston, TX have shown that wastewater SARS-CoV-2 viral loads strongly correlate with trends from multiple disease indicators, such as COVID-19 positivity rate, emergency department visit rate, and hospital bed usage rate.
In an 86-week surveillance study, public health leaders and academic researchers from the Houston Health Department, Houston Public Works and Rice University, collected and measured SARS-CoV-2 viral concentrations through 24-hour samples from across 39 wastewater treatment plants over three major COVID-19 surges. The study chronicled Alpha, Delta, and Omicron infection waves in near real-time from September 1, 2020 to April 25, 2022.
The study, which was published online in the journal Science of the Total Environment on September 24, posits that wastewater information must be triangulated with other disease surveillance systems for it to be integrated and used as a routine public health metric.
Lauren Stadler, an assistant professor of civil and environmental engineering at Rice University, is lead author on the paper.
Stadler’s lab has collaborated with the Houston Health Department lab to provide weekly measurements from 39 city-owned wastewater treatment plants, which serve more than 2 million people. These weekly measurements form the basis of an ongoing real-time tracking system for informed responses to viral outbreaks and to prevent illness. In addition to these sites, samples have been collected at lift stations around the city, schools, nursing homes and jails. A total of about 100 locations have been sampled every week.
Data from the wastewater monitoring program has been summarized in weekly reports that provide information about the virus at sewershed, zip code, and manhole levels. These reports are shared weekly with city and health department officials and Dr. David Persse, Houston’s chief medical officer. Dr. Persse has also been a key contributor to the wastewater program.
“The strong correlation between disease indicators and wastewater viral loads demonstrates that wastewater is a powerful tool for providing fast, accurate surveillance information of disease outbreaks and trends,” said Loren Hopkins, who is the chief environmental science officer for the Houston Health Department, a professor in the practice of statistics at Rice and Houston Wastewater Epidemiology project team lead.
“Public health surveillance systems are multifaceted, therefore more work needs to be done to optimize detection, clarify how wastewater data should be synthesized with other public health data and to bridge communication gaps. This is especially important for major international cities,” added Hopkins.
As the chief environmental science officer for the Houston Health Department, Hopkins worked with project collaborators to design, implement and maintain the active wastewater monitoring system for Houston.
Because Houston’s wastewater system includes numerous zoned wastewater treatment plants, sampling from each site allows for information on localized hotspots to provide early warning to areas needing interventions.
For example, during the first wave of the pandemic, the 69th Street Wastewater Treatment Plant, which is the city’s largest facility, had earlier increases in weekly percent change in viral loads than the city-wide total. More importantly, three neighborhood hot spots led the citywide total across all three COVID-19 waves: Beltway, Chocolate Bayou, and Intercontinental Airport.
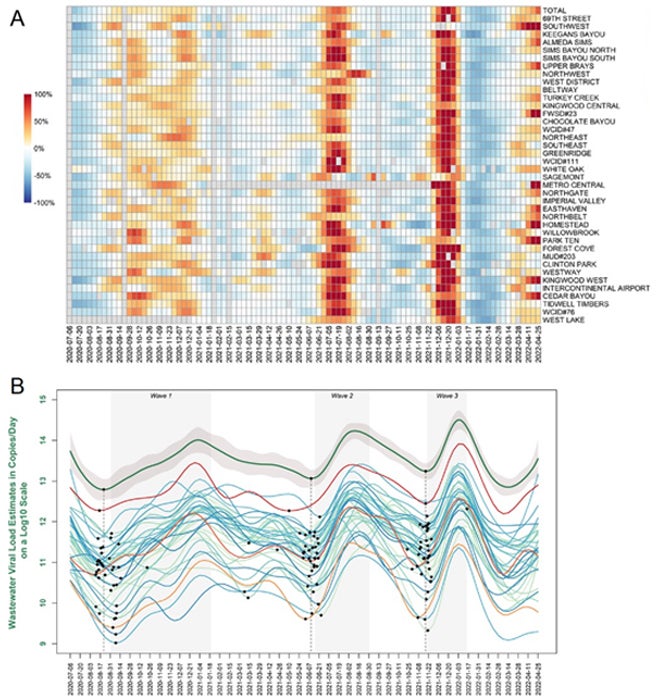
“The Houston study results confirm that ongoing analysis of highly trafficked areas, such as Intercontinental Airport, will serve as a sentinel for early detection of infection surges,” said Katherine Ensor, the Noah G. Harding Professor of Statistics.
Ensor has worked with analysts at Rice and the Houston Health Department to lead the development of an intensive statistical system that uses spatial sampling, along with temporal sampling, to quantify and assess trends in viral prevalence in near real-time.
Cross-correlation analysis was used to assess leading or lagging relationships between the wastewater viral load and other metrics, which were found to shift over the three waves of the pandemic.
Since January 2021, the weekly analysis has been performed by co-author Rebecca Schneider of the Houston Health Department, an alumnus of the university’s Professional Master of Statistics program. Ensor and Schneider ensure the system is working as planned and perform additional research to understand emerging issues.
Ongoing collaborative efforts to further establish multiple wastewater surveillance methods for routine metrics include assessing the optimal sampling frequency and sample locations and taking steps to better understand and minimize the factors contributing to measurement variability. Training initiatives are also underway in both wastewater epidemiology and in efforts to incorporate wastewater surveillance information into existing systems used by local, state, federal, and international systems.
Additional co-authors on the paper include Camille McCall, a postdoctoral research associate in civil and environmental engineering at Rice, and Houston Health Department analyst Kelsey Caton who contributed to the statistical analysis for the paper.
Shawn Hutchins, Communications Specialist

